Bcbs Clinical Appeal Form
Bcbs Clinical Appeal Form - When not to submit an appeal. Web the provider clinical appeal form should be used when clinical decision making is necessary: Medical claims, vision claims and reimbursement forms, prescription drug forms, coverage and premium payment and personal information. Web electronic clinical claim appeal request via availity ® the dispute tool allows providers to electronically submit appeal requests for specific clinical claim denials through the availity portal. Web appeals must be submitted within one year from the date on the remittance advice. Please send only one claim per form. Check the “utilization management” box under appeal type; Utilization management adverse determination coding and payment rule please review the instructions for each category below to ensure proper routing of your appeal. Web florida blue members can access a variety of forms including: When to submit an appeal.
Web the provider clinical appeal form should be used when clinical decision making is necessary: When applicable, the dispute option is. Please review the instructions for each category below to ensure proper routing of your appeal. Bcn advantage appeals and grievance unit p.o. Check the appropriate box for the utilization management appeal reason, either “authorization” or “precertification”; Date _____ provider reconsideration administrative appeal (must include reconsideration #) _____ reason for provider reconsideration request / administrative appeal (check one) claim allowance Review is conducted by a physician. When not to submit an appeal. Web florida blue members can access a variety of forms including: Medical claims, vision claims and reimbursement forms, prescription drug forms, coverage and premium payment and personal information.
Date _____ provider reconsideration administrative appeal (must include reconsideration #) _____ reason for provider reconsideration request / administrative appeal (check one) claim allowance Web a clinical appeal is a request to change an adverse determination for care or services that were denied on the basis of lack of medical necessity, or when services are determined to be experimental, investigational or cosmetic. Web the provider clinical appeal form should be used when clinical decision making is necessary: Utilization management adverse determination coding and payment rule please review the instructions for each category below to ensure proper routing of your appeal. When not to submit an appeal. When to submit an appeal. Web florida blue members can access a variety of forms including: Check the “utilization management” box under appeal type; Bcn advantage appeals and grievance unit p.o. Web appeals must be submitted within one year from the date on the remittance advice.
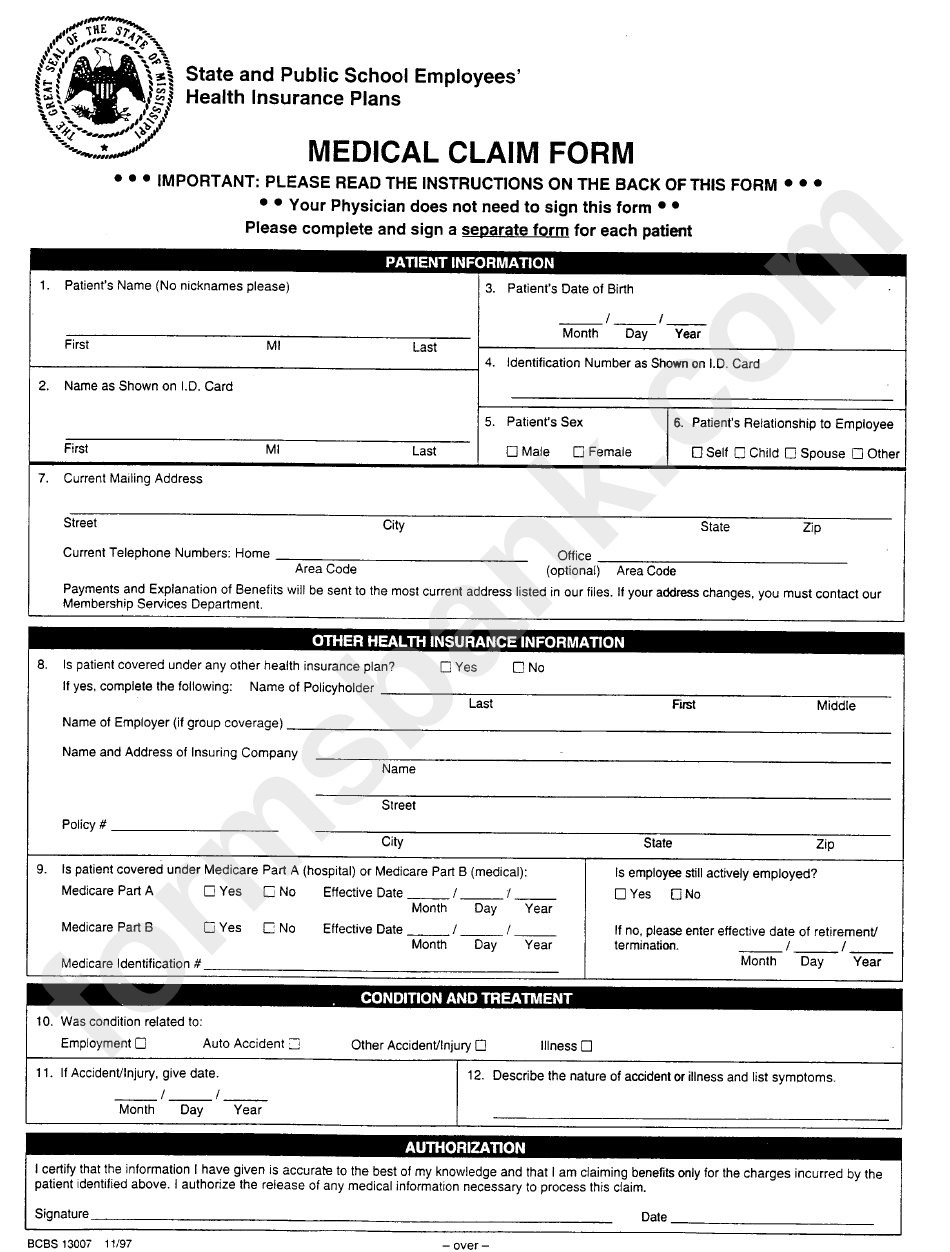
Form Bcbs 13007 State And Public School Employees Medical Claim Form
When to submit an appeal. Review is conducted by a physician. Appeals are divided into two categories: And enter the authorization or precertification. Date _____ provider reconsideration administrative appeal (must include reconsideration #) _____ reason for provider reconsideration request / administrative appeal (check one) claim allowance
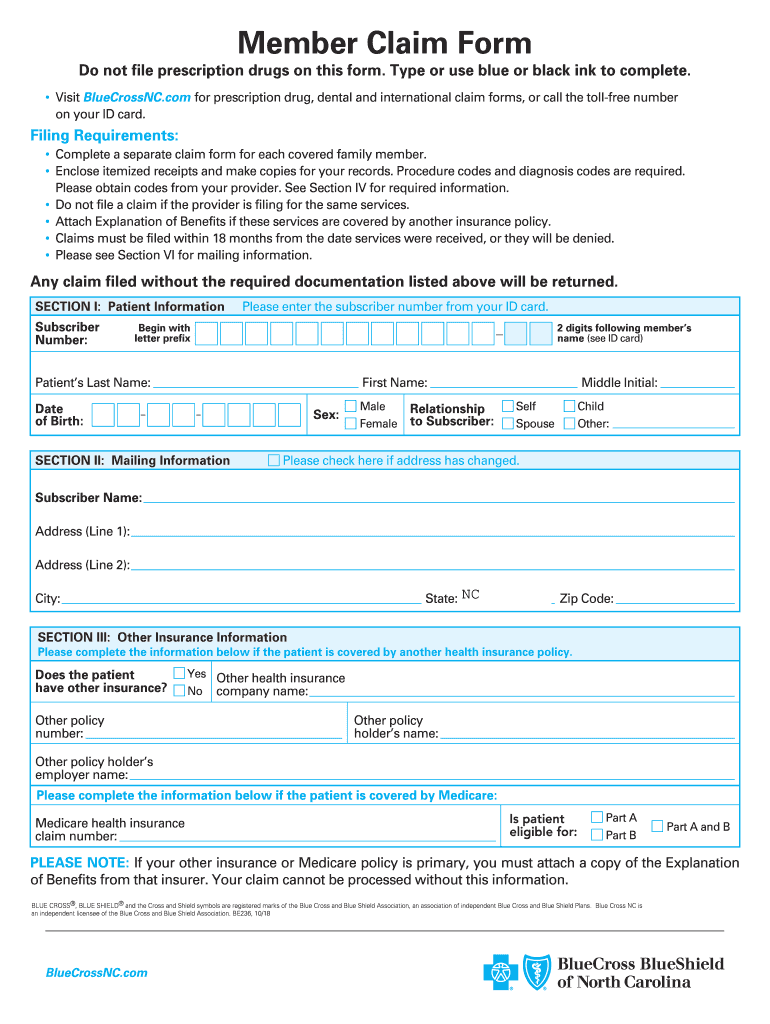
Nc Bcbs Form Fill Out and Sign Printable PDF Template signNow
Appeals are divided into two categories: When to submit an appeal. Web appeals must be submitted within one year from the date on the remittance advice. Web florida blue members can access a variety of forms including: Please review the instructions for each category below to ensure proper routing of your appeal.
TN BCBS 17PED153727 20172021 Fill and Sign Printable Template Online
Check the “utilization management” box under appeal type; When not to submit an appeal. Web provider appeal form instructions physicians and providers may appeal how a claim processed, paid or denied. Check the appropriate box for the utilization management appeal reason, either “authorization” or “precertification”; Web a clinical appeal is a request to change an adverse determination for care or.
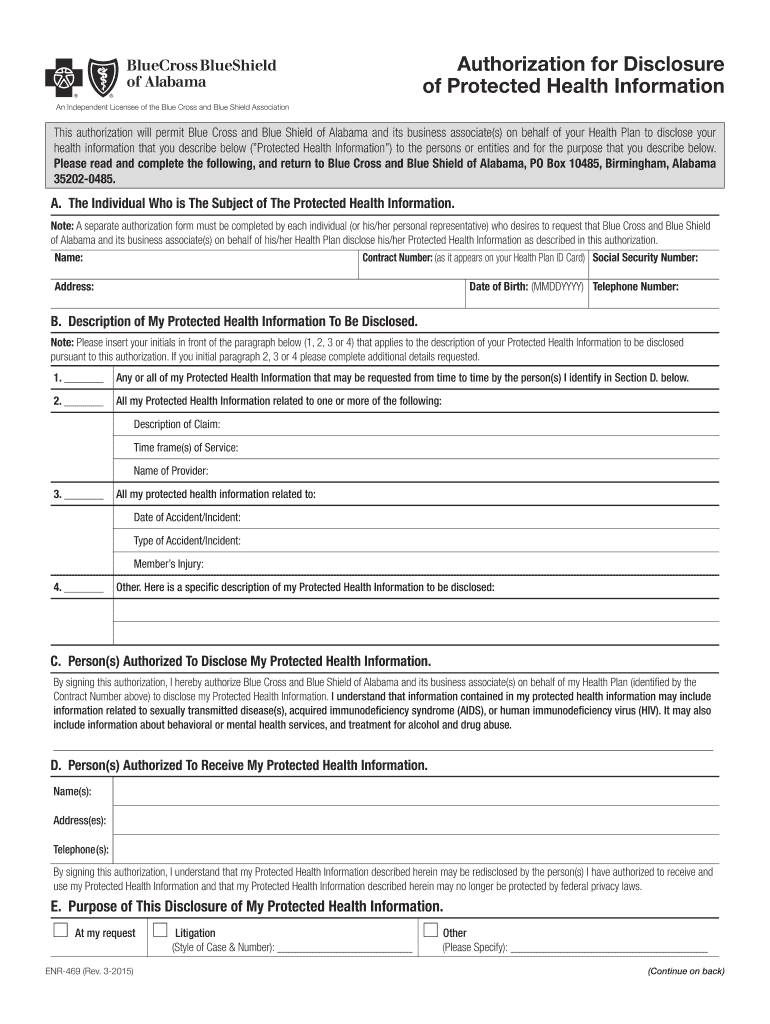
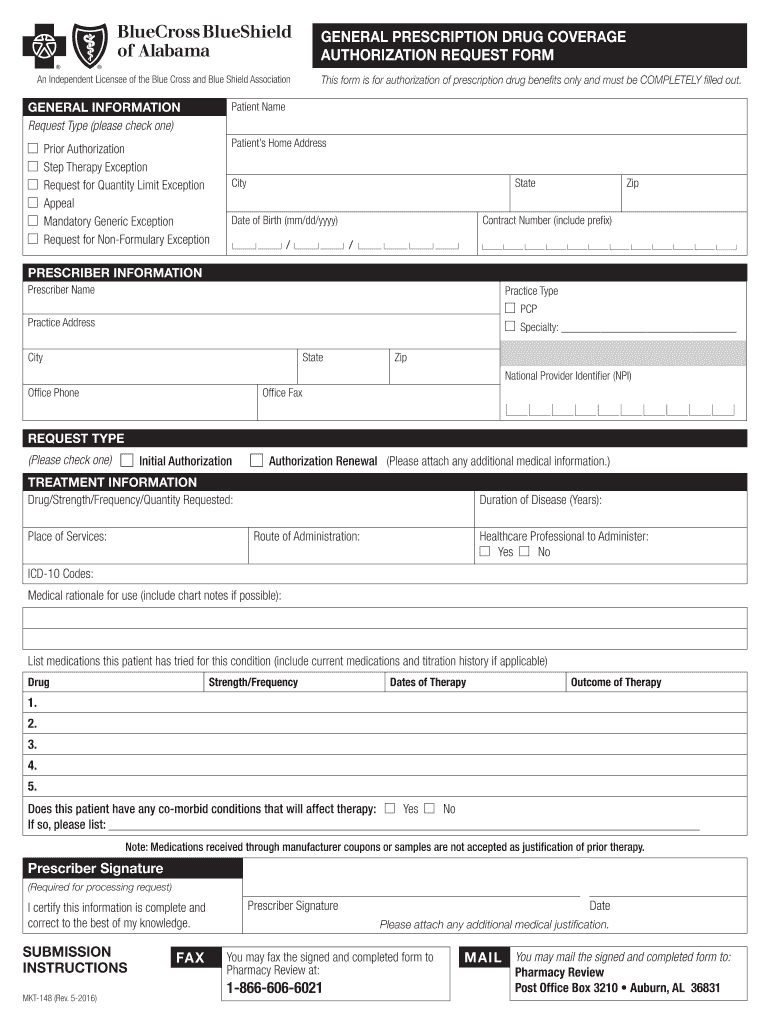
Bcbs Of Alabama Prior Authorization Fill Out and Sign Printable PDF
Bcn advantage appeals and grievance unit p.o. Please send only one claim per form. When to submit an appeal. Web the provider clinical appeal form should be used when clinical decision making is necessary: Web florida blue members can access a variety of forms including:
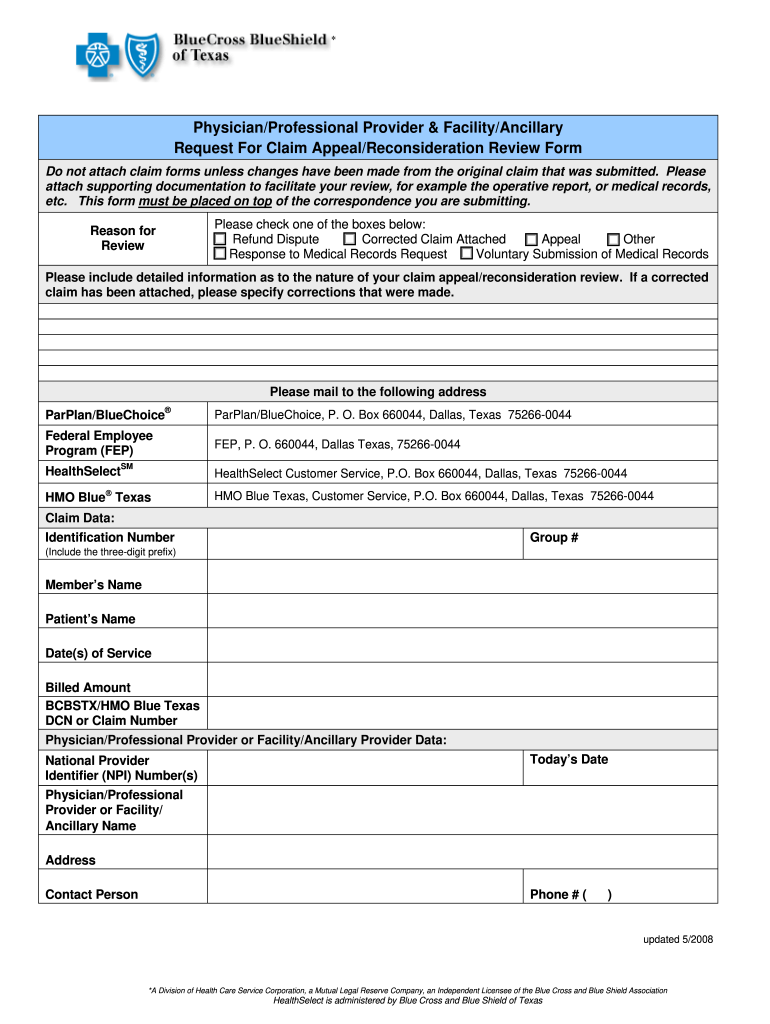
Texas Bcbs Provider Appeal Fill Out and Sign Printable PDF Template
Web appeals must be submitted within one year from the date on the remittance advice. Bcn advantage appeals and grievance unit p.o. And enter the authorization or precertification. Appeals are divided into two categories: Utilization management adverse determination coding and payment rule please review the instructions for each category below to ensure proper routing of your appeal.
Bcbs Federal Provider Appeal form Best Of Fep Prior Authorization form â
Review is conducted by a physician. Web the provider clinical appeal form should be used when clinical decision making is necessary: Please review the instructions for each category below to ensure proper routing of your appeal. When not to submit an appeal. Web electronic clinical claim appeal request via availity ® the dispute tool allows providers to electronically submit appeal.
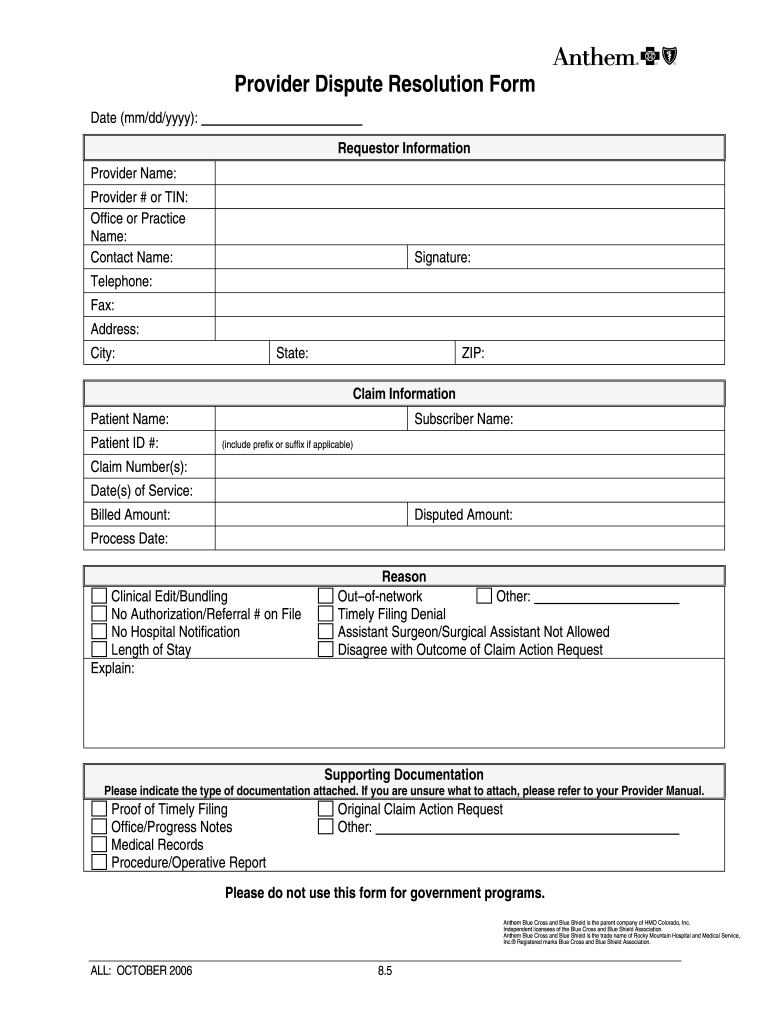
Anthem provider dispute form Fill out & sign online DocHub
Appeals are divided into two categories: Web florida blue members can access a variety of forms including: Check the appropriate box for the utilization management appeal reason, either “authorization” or “precertification”; Medical claims, vision claims and reimbursement forms, prescription drug forms, coverage and premium payment and personal information. Web a clinical appeal is a request to change an adverse determination.
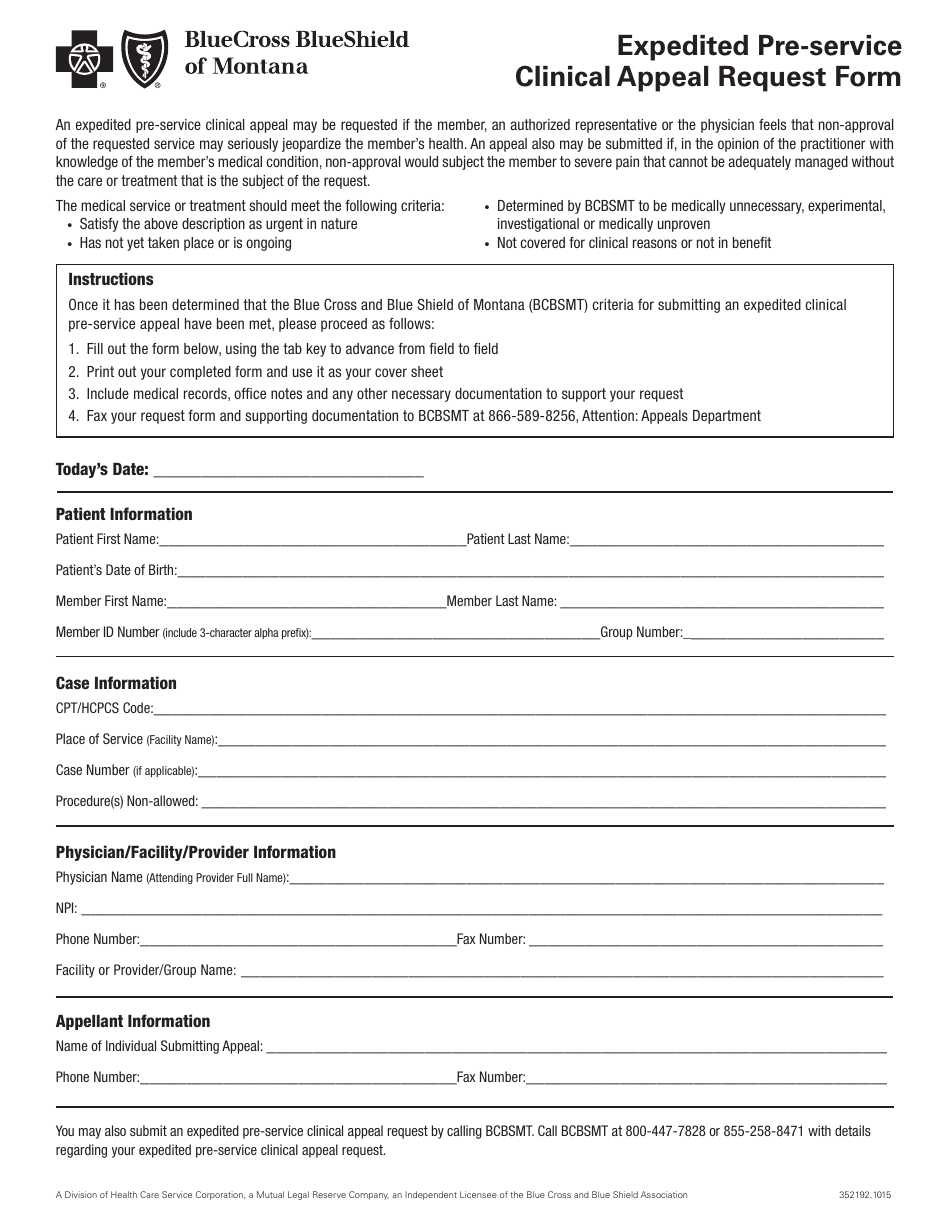
Form 352192.1015 Download Fillable PDF or Fill Online Expedited Pre
Please review the instructions for each category below to ensure proper routing of your appeal. Review is conducted by a physician. When applicable, the dispute option is. Web a clinical appeal is a request to change an adverse determination for care or services that were denied on the basis of lack of medical necessity, or when services are determined to.
Bcbs Alabama Prior Authorization Form Fill Out and Sign Printable PDF
Please send only one claim per form. Web a clinical appeal is a request to change an adverse determination for care or services that were denied on the basis of lack of medical necessity, or when services are determined to be experimental, investigational or cosmetic. And enter the authorization or precertification. When applicable, the dispute option is. Web provider appeal.
Bcbs Federal Provider Appeal form Elegant Service Dog Letter Template
Review is conducted by a physician. Bcn advantage appeals and grievance unit p.o. And enter the authorization or precertification. When to submit an appeal. Utilization management adverse determination coding and payment rule please review the instructions for each category below to ensure proper routing of your appeal.
Review Is Conducted By A Physician.
Web provider appeal form instructions physicians and providers may appeal how a claim processed, paid or denied. Check the “utilization management” box under appeal type; Web a clinical appeal is a request to change an adverse determination for care or services that were denied on the basis of lack of medical necessity, or when services are determined to be experimental, investigational or cosmetic. Web appeals must be submitted within one year from the date on the remittance advice.
Please Review The Instructions For Each Category Below To Ensure Proper Routing Of Your Appeal.
Please send only one claim per form. When not to submit an appeal. And enter the authorization or precertification. Web the provider clinical appeal form should be used when clinical decision making is necessary:
Appeals Are Divided Into Two Categories:
Medical claims, vision claims and reimbursement forms, prescription drug forms, coverage and premium payment and personal information. When applicable, the dispute option is. Utilization management adverse determination coding and payment rule please review the instructions for each category below to ensure proper routing of your appeal. When to submit an appeal.
Check The Appropriate Box For The Utilization Management Appeal Reason, Either “Authorization” Or “Precertification”;
Web florida blue members can access a variety of forms including: Bcn advantage appeals and grievance unit p.o. Web electronic clinical claim appeal request via availity ® the dispute tool allows providers to electronically submit appeal requests for specific clinical claim denials through the availity portal. Date _____ provider reconsideration administrative appeal (must include reconsideration #) _____ reason for provider reconsideration request / administrative appeal (check one) claim allowance