Bcbs Provider Appeal Form
Bcbs Provider Appeal Form - Most provider appeal requests are related to a length of stay or treatment setting denial. Check the “utilization management” box under appeal type; As part of the process, you'll have to fill out the above form. Web use this form to submit appeal requests for their commercial and bluecare patients. You can find this and the other requirements for an appeal at the centers for medicare & medicaid services. And enter the authorization or precertification number. Fields with an asterisk (*) are required. Access and download these helpful bcbstx health care provider forms. Please submit only one claim adjustment, status check or appeal per page and mail with appropriate attachments to blue cross. Web provider forms & guides.
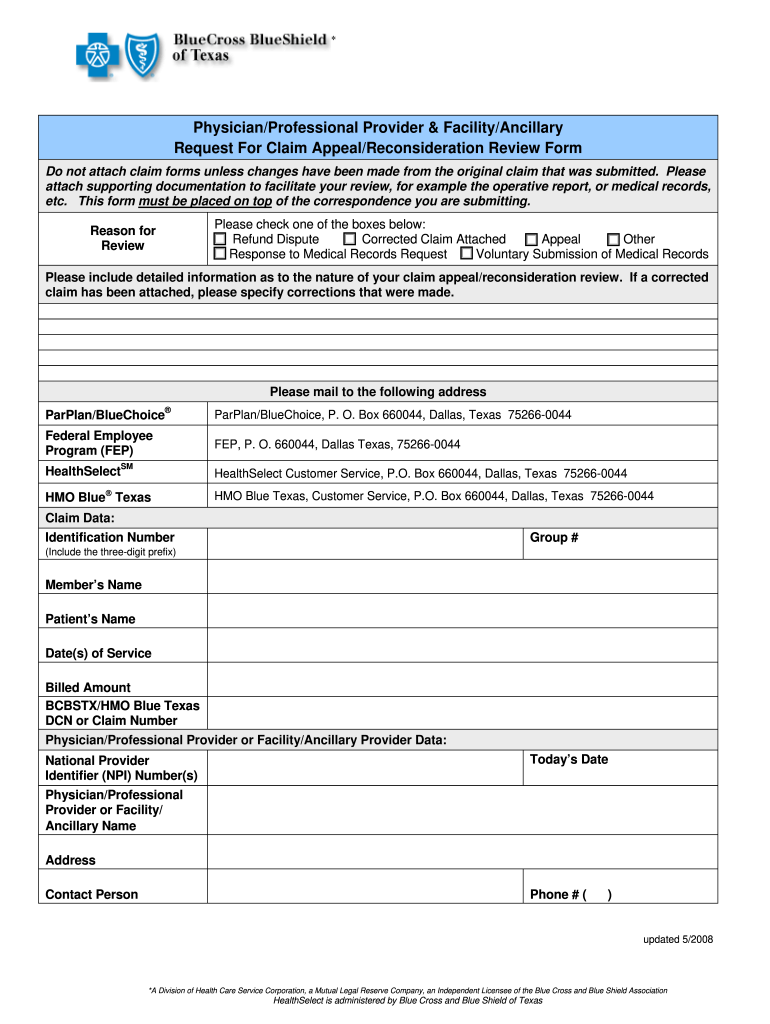
You can find this and the other requirements for an appeal at the centers for medicare & medicaid services. And enter the authorization or precertification number. Check the appropriate box for the utilization management appeal reason, either “authorization” or “precertification”; Web level i provider appeals for billing/coding disputes and medical necessity determinations should be submitted by sending a written request for appeal using the level i provider appeal form which is available online. Web blue cross blue shield of texas is committed to giving health care providers with the support and assistance they need. Web provider appeal request form provider appeal request form please complete one form per member to request an appeal of an adjudicated/paid claim. Be specific when completing the “description of appeal” and “expected outcome.” please provider all supporting documents with submitted appeal. Web provider claim adjustment / status check / appeal form instructions blue cross blue shield of minnesota and blue plus the general instructions are listed below. Most provider appeal requests are related to a length of stay or treatment setting denial. Please submit only one claim adjustment, status check or appeal per page and mail with appropriate attachments to blue cross.
Fields with an asterisk (*) are required. Most provider appeal requests are related to a length of stay or treatment setting denial. Web provider appeal request form provider appeal request form please complete one form per member to request an appeal of an adjudicated/paid claim. Be specific when completing the “description of appeal” and “expected outcome.” please provider all supporting documents with submitted appeal. You can find this and the other requirements for an appeal at the centers for medicare & medicaid services. Web level i provider appeals for billing/coding disputes and medical necessity determinations should be submitted by sending a written request for appeal using the level i provider appeal form which is available online. This is different from the request for claim review request process outlined above. Check the appropriate box for the utilization management appeal reason, either “authorization” or “precertification”; Web use this form to submit appeal requests for their commercial and bluecare patients. Web provider claim adjustment / status check / appeal form instructions blue cross blue shield of minnesota and blue plus the general instructions are listed below.
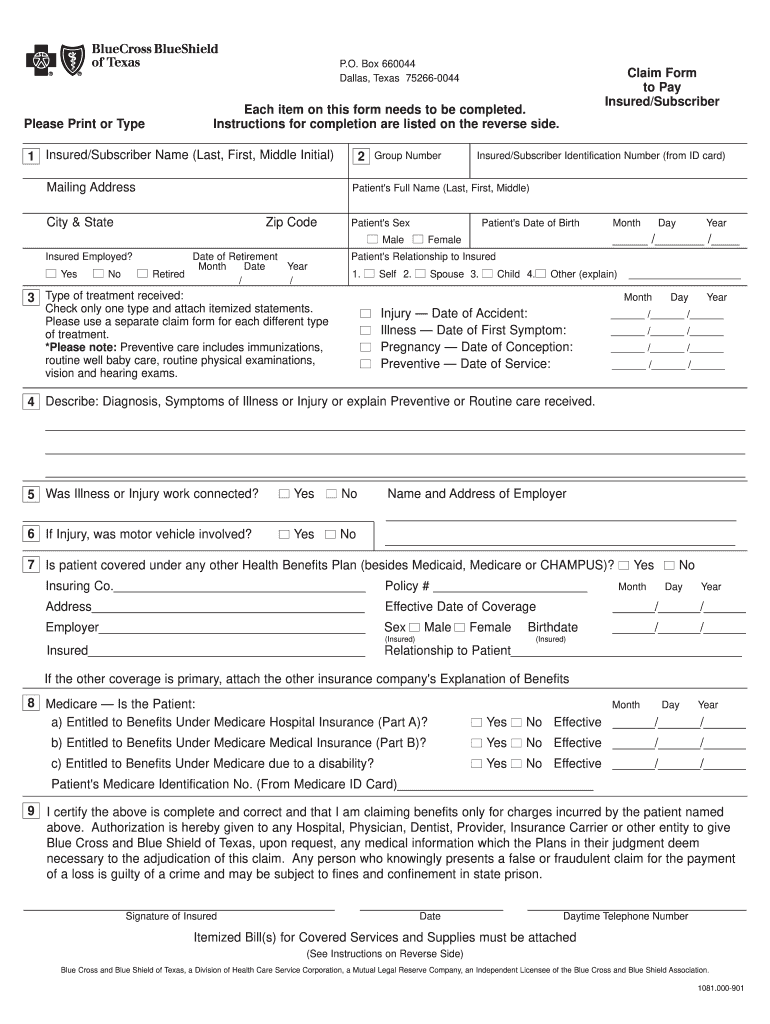
Bcbs Claim Form Fill Out and Sign Printable PDF Template signNow
Web a provider appeal is an official request for reconsideration of a previous denial issued by the bcbsil medical management area. Web level i provider appeals for billing/coding disputes and medical necessity determinations should be submitted by sending a written request for appeal using the level i provider appeal form which is available online. Fields with an asterisk (*) are.
Bcbs Federal Provider Appeal form Best Of File Plaint Blue Shield
Be specific when completing the “description of appeal” and “expected outcome.” please provider all supporting documents with submitted appeal. Check the “utilization management” box under appeal type; Web a provider appeal is an official request for reconsideration of a previous denial issued by the bcbsil medical management area. Web provider claim adjustment / status check / appeal form instructions blue.
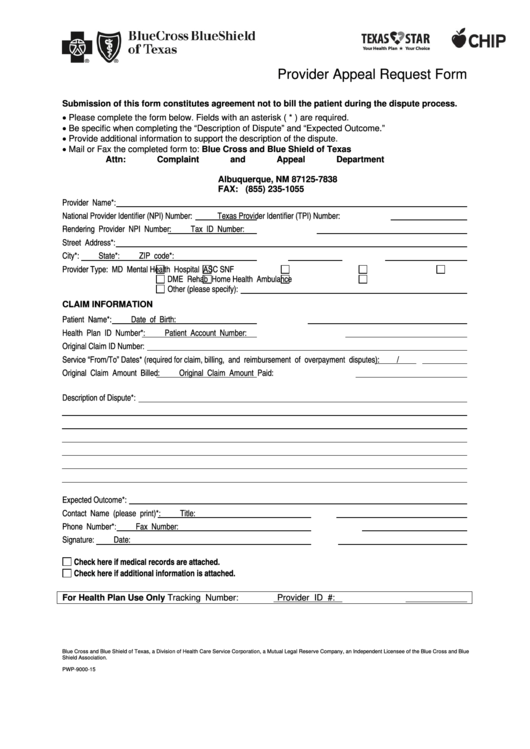
Texas Bcbs Provider Appeal Fill Out and Sign Printable PDF Template
Web use this form to submit appeal requests for their commercial and bluecare patients. If you have a problem with your blue cross blue shield of michigan service, you can use this form to file an appeal with us. Fields with an asterisk (*) are required. Web provider appeal request form provider appeal request form please complete one form per.
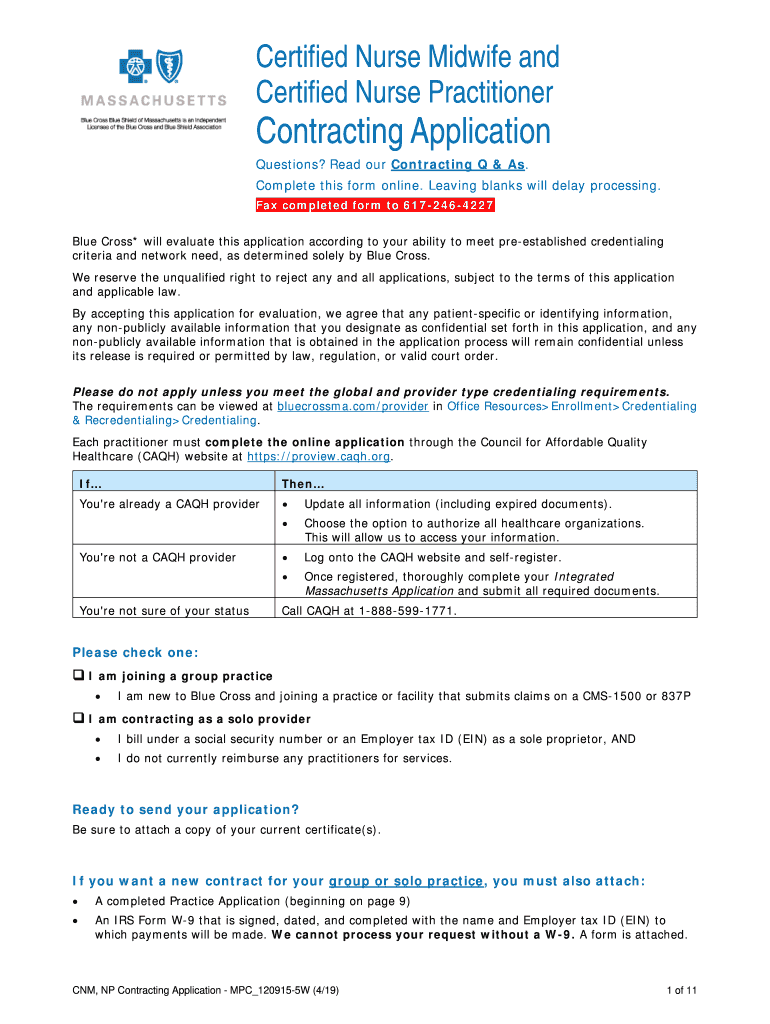
MA BCBS MPC_1209155W 20202021 Fill and Sign Printable Template
Web appeal form who is this for? This is different from the request for claim review request process outlined above. Web provider forms & guides. If you have a problem with your blue cross blue shield of michigan service, you can use this form to file an appeal with us. Web provider claim adjustment / status check / appeal form.
BCBS in Provider Dispute Resolution Request Form Blue Cross Blue
Web use this form to submit appeal requests for their commercial and bluecare patients. Web provider appeal request form provider appeal request form please complete one form per member to request an appeal of an adjudicated/paid claim. If you're a blue cross blue shield of michigan member and are unable to resolve your concern through customer service, we have a.
Bluecross Blueshield Of Texas Provider Appeal Request Form printable
Most provider appeal requests are related to a length of stay or treatment setting denial. Web level i provider appeals for billing/coding disputes and medical necessity determinations should be submitted by sending a written request for appeal using the level i provider appeal form which is available online. Access and download these helpful bcbstx health care provider forms. Web provider.
VT BCBS PA.PC.RR 20122021 Fill and Sign Printable Template Online
Web provider claim adjustment / status check / appeal form instructions blue cross blue shield of minnesota and blue plus the general instructions are listed below. Fields with an asterisk (*) are required. Web level i provider appeals for billing/coding disputes and medical necessity determinations should be submitted by sending a written request for appeal using the level i provider.
TN BCBS 17PED153727 20172021 Fill and Sign Printable Template Online
Web provider claim adjustment / status check / appeal form instructions blue cross blue shield of minnesota and blue plus the general instructions are listed below. And enter the authorization or precertification number. You can find this and the other requirements for an appeal at the centers for medicare & medicaid services. Web appeal form who is this for? Please.
Bcbs Federal Provider Appeal form New Blue Cross Of Mass Giving Opioid
Web provider claim adjustment / status check / appeal form instructions blue cross blue shield of minnesota and blue plus the general instructions are listed below. Easily find and download forms, guides, and other related documentation that you need to do business with anthem all in one convenient location! This is different from the request for claim review request process.
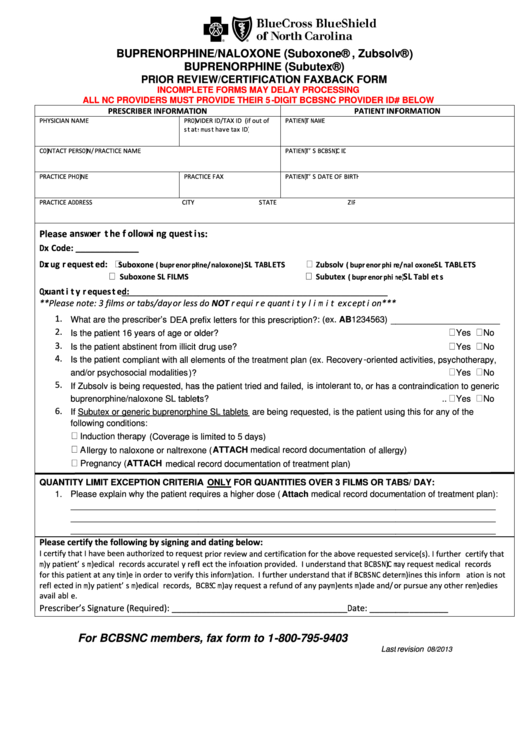
Bcbsnc Prior Review/certification Faxback Form printable pdf download
Web level i provider appeals for billing/coding disputes and medical necessity determinations should be submitted by sending a written request for appeal using the level i provider appeal form which is available online. Web provider forms & guides. Check the appropriate box for the utilization management appeal reason, either “authorization” or “precertification”; Be specific when completing the “description of appeal”.
Fields With An Asterisk (*) Are Required.
As part of the process, you'll have to fill out the above form. If you have a problem with your blue cross blue shield of michigan service, you can use this form to file an appeal with us. You can find this and the other requirements for an appeal at the centers for medicare & medicaid services. Web blue cross blue shield of texas is committed to giving health care providers with the support and assistance they need.
This Is Different From The Request For Claim Review Request Process Outlined Above.
Easily find and download forms, guides, and other related documentation that you need to do business with anthem all in one convenient location! Web provider appeal request form provider appeal request form please complete one form per member to request an appeal of an adjudicated/paid claim. Be specific when completing the “description of appeal” and “expected outcome.” please provider all supporting documents with submitted appeal. Web a provider appeal is an official request for reconsideration of a previous denial issued by the bcbsil medical management area.
And Enter The Authorization Or Precertification Number.
Web level i provider appeals for billing/coding disputes and medical necessity determinations should be submitted by sending a written request for appeal using the level i provider appeal form which is available online. Web provider forms & guides. Web use this form to submit appeal requests for their commercial and bluecare patients. Access and download these helpful bcbstx health care provider forms.
Check The Appropriate Box For The Utilization Management Appeal Reason, Either “Authorization” Or “Precertification”;
If you're a blue cross blue shield of michigan member and are unable to resolve your concern through customer service, we have a formal grievance and appeals process. Web provider claim adjustment / status check / appeal form instructions blue cross blue shield of minnesota and blue plus the general instructions are listed below. Most provider appeal requests are related to a length of stay or treatment setting denial. Web appeal form who is this for?