Blue Cross Appeals Form
Blue Cross Appeals Form - Complete the form and mail it to the address shown on the back. Web submit an appeal, send us a completed request for claim review form. Web authorized representative) in order for a provider to appeal on their behalf. Web mail the completed form and appeal request to: State health plan ppo ; If coverage or payment for an item or medical service is denied that you think should be covered. Bcbsks must make mail your appeal to: This is due within one year of the date the claim was denied. Web if there is a full or partial claim rejection or the payment is not the amount expected, submit a claims appeal. By mail or by fax:.
Web mail the completed form to: State health plan ppo ; Print the complaint or appeal form (below) for your medicare health plan. Web filing a medical appeal. You can submit up to two appeals for the. Web submit an appeal, send us a completed request for claim review form. You may file an appeal in writing by. The appeal must be received by anthem blue cross (anthem) within 365. Download an electronic copy of the blue cross nc member appeal. Web to file a grievance, you may complete this form, or you may write a letter outlining as many details as possible regarding the incident in question.
Print the complaint or appeal form (below) for your medicare health plan. Web provider appeal form please complete the following information and return this form with supporting documentation to the applicable address listed on the corresponding appeal. Web authorized representative) in order for a provider to appeal on their behalf. Call the bcbstx customer advocate department. Download an electronic copy of the blue cross nc member appeal. The appeal must be received by anthem blue cross (anthem) within 365. You may file an appeal in writing by. Web english authorized representative designation form use this form to select an individual or entity to act on your behalf during the disputed claims process. Web mail the completed form to: Your completed form or letter can.
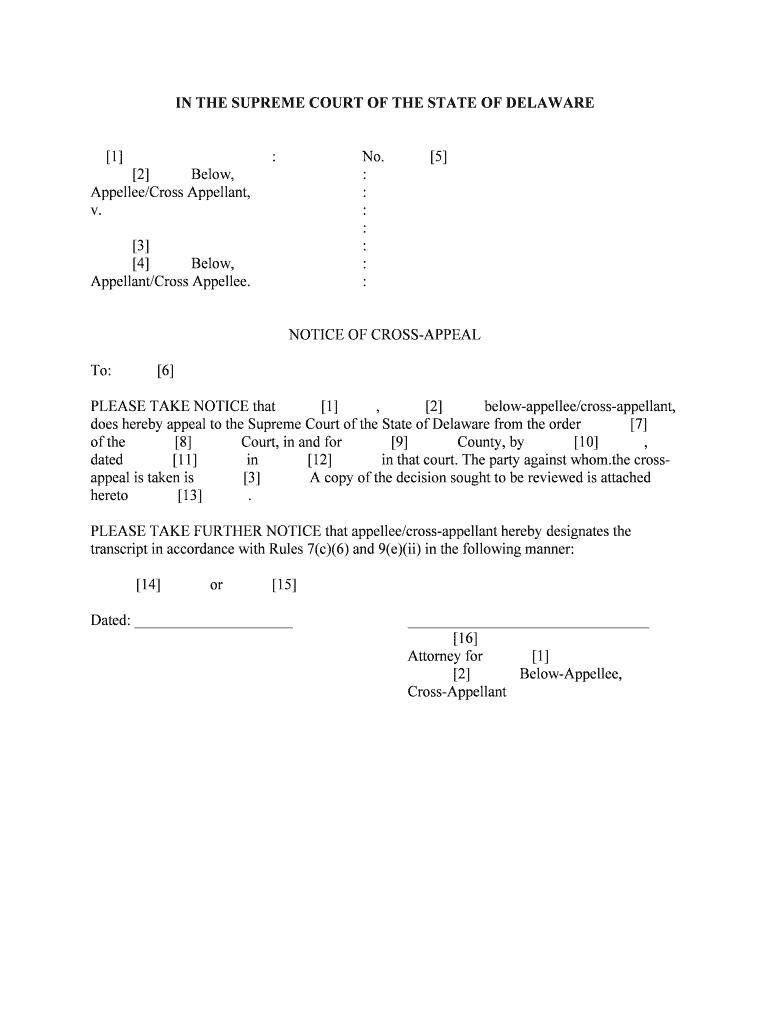
Rule 28 1 Cross Appeals Fourth Circuit Court of Appeals Form Fill Out
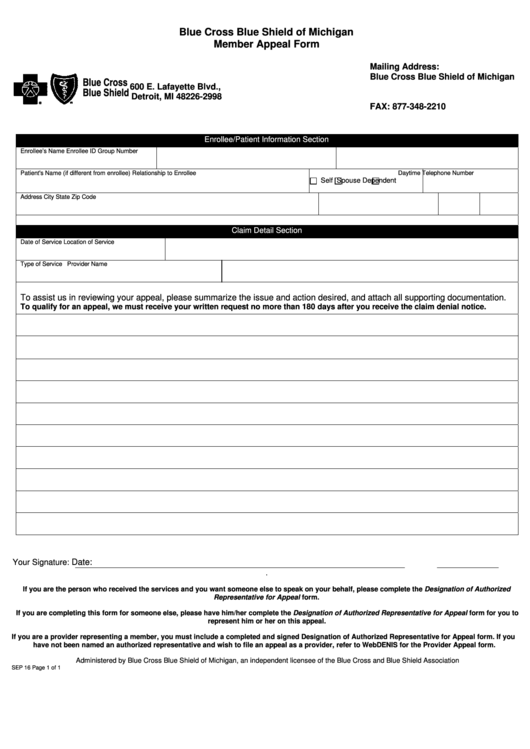
If coverage or payment for an item or medical service is denied that you think should be covered. If you have a problem with your blue cross blue shield of michigan service, you can use this form to file an appeal with us. Mail or fax it to us using the address or fax number listed at the top of.
Blue Cross Blue Shield Overseas Claim Form Fill Online, Printable
Bcbsks must make mail your appeal to: If you have a problem with your blue cross blue shield of michigan service, you can use this form to file an appeal with us. Web english authorized representative designation form use this form to select an individual or entity to act on your behalf during the disputed claims process. Web po box.
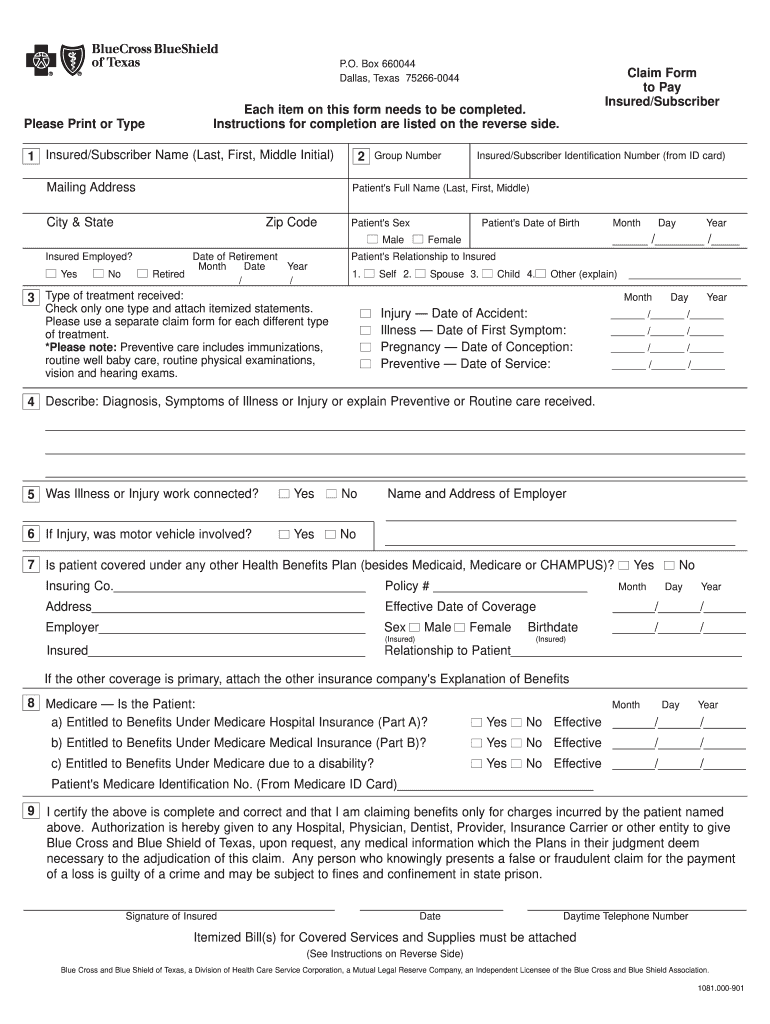
Bcbs Claim Form Fill Out and Sign Printable PDF Template signNow
Print the complaint or appeal form (below) for your medicare health plan. Web blue cross and blue shield of kansas (bcbsks) must receive your appeal within 180 days of the adverse decision. Web filing a medical appeal. If coverage or payment for an item or medical service is denied that you think should be covered. The appeal must be received.
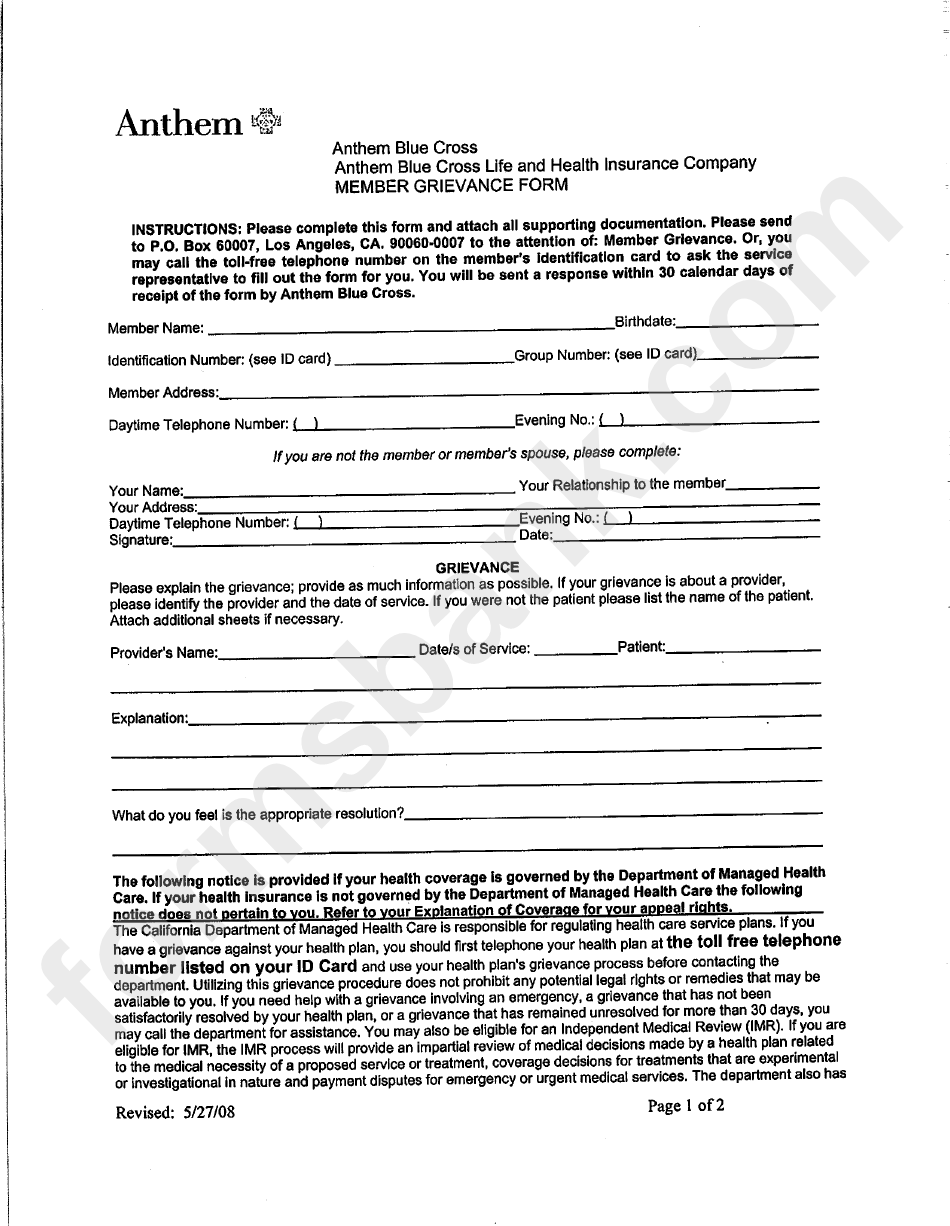
Anthem Provider Dispute Resolution Form Colorado Fill Online
State health plan ppo ; By mail or by fax:. If you have a problem with your blue cross blue shield of michigan service, you can use this form to file an appeal with us. Web if there is a full or partial claim rejection or the payment is not the amount expected, submit a claims appeal. If you are.
Wellcare Medicare Prior Authorization Forms
This is due within one year of the date the claim was denied. The appeal must be received by anthem blue cross (anthem) within 365. Web appeal form who is this for? Web blue cross and blue shield of kansas (bcbsks) must receive your appeal within 180 days of the adverse decision. Web if there is a full or partial.
Anthem Blue Cross Member Grievance Form printable pdf download
You can submit up to two appeals for the. Once the authorization is signed and dated, the provider will need to fax or mail the form and. By mail or by fax:. Web mail the completed form and appeal request to: This is due within one year of the date the claim was denied.
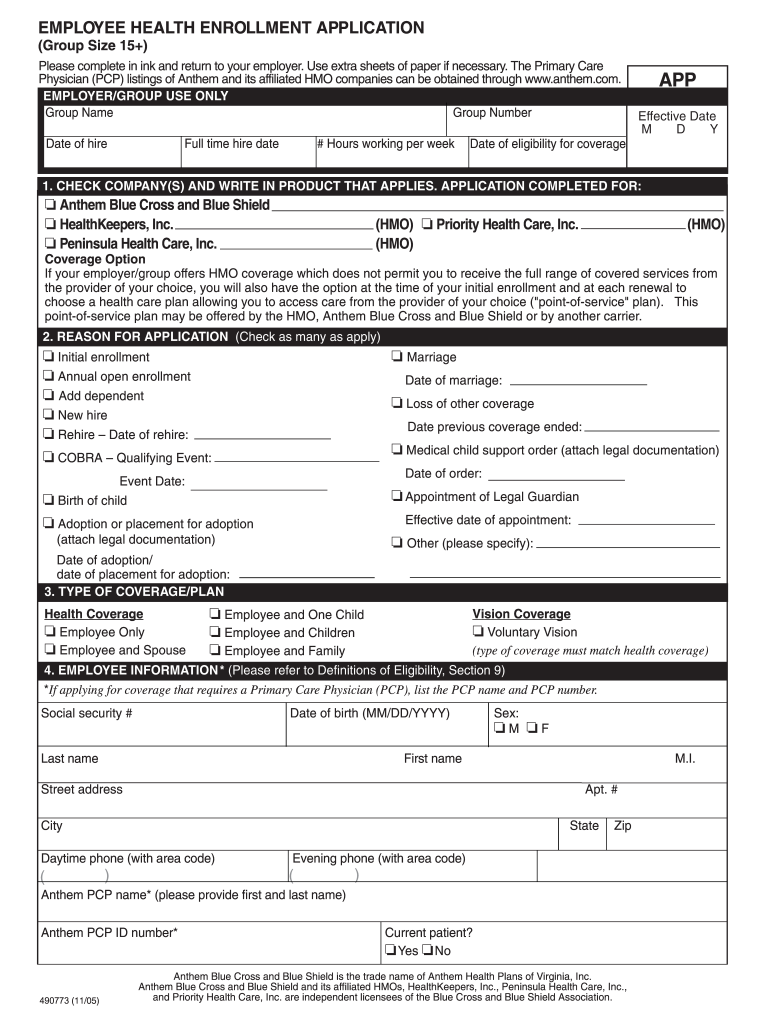
Anthem Enrollment Application Fill Out and Sign Printable PDF
State health plan ppo ; Web if there is a full or partial claim rejection or the payment is not the amount expected, submit a claims appeal. If you're a blue cross. Complete the form and mail it to the address shown on the back. You can ask for an appeal:
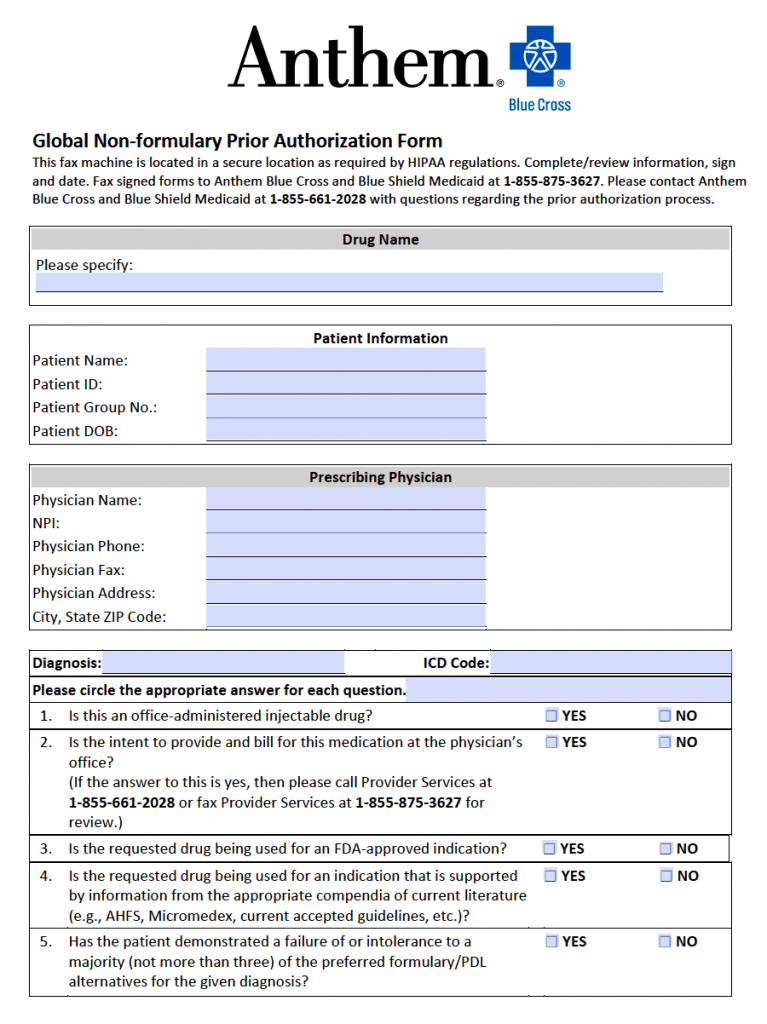
Free Anthem Blue Cross / Blue Shield Prior Prescription (Rx
By mail or by fax:. This is due within one year of the date the claim was denied. Once the authorization is signed and dated, the provider will need to fax or mail the form and. Web appeal form who is this for? Web submit an appeal, send us a completed request for claim review form.
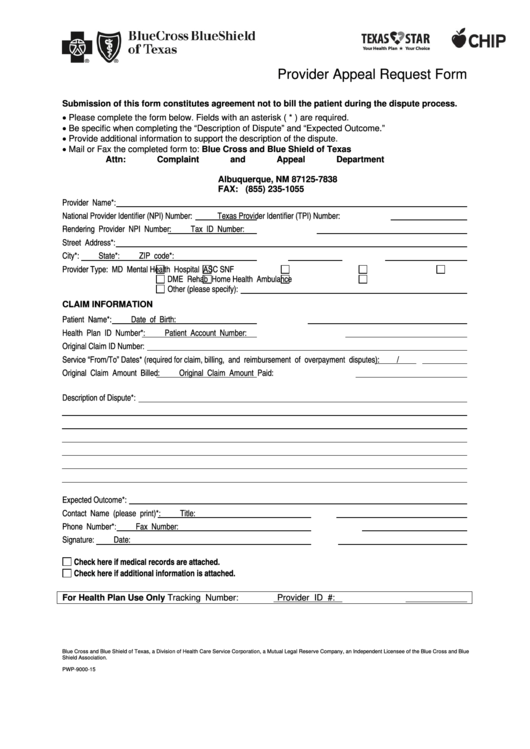
Bluecross Blueshield Of Texas Provider Appeal Request Form printable
Web appeal form who is this for? Web • request an appeal if you feel we didn’t cover or pay enough for a service or drug you received. Your completed form or letter can. You may file an appeal in writing by. You can ask for an appeal if coverage or payment for an item or medical service is denied.
Fillable Blue Cross Blue Shield Of Michigan Member Appeal Form
Your completed form or letter can. • request a grievance if you have a complaint against blue cross or your. Web mail the completed form to: If coverage or payment for an item or medical service is denied that you think should be covered. Web • request an appeal if you feel we didn’t cover or pay enough for a.
If You Are Unable To.
Print the complaint or appeal form (below) for your medicare health plan. Download an electronic copy of the blue cross nc member appeal. Web mail the completed form and appeal request to: You can submit up to two appeals for the.
Call The Bcbstx Customer Advocate Department.
Complete the form and mail it to the address shown on the back. State health plan ppo ; If coverage or payment for an item or medical service is denied that you think should be covered. Web if you'd like to make a complaint or file an appeal about a claim that was denied, call customer service at the number on the back of your member id card.
Bcbsks Must Make Mail Your Appeal To:
If you have a problem with your blue cross blue shield of michigan service, you can use this form to file an appeal with us. The appeal must be received by anthem blue cross (anthem) within 365. Mail or fax it to us using the address or fax number listed at the top of the form. Web • request an appeal if you feel we didn’t cover or pay enough for a service or drug you received.
Web To File A Grievance, You May Complete This Form, Or You May Write A Letter Outlining As Many Details As Possible Regarding The Incident In Question.
By mail or by fax:. Web mail the completed form to: You can ask for an appeal if coverage or payment for an item or medical service is denied that you think should be covered. Web level i provider appeals for billing/coding disputes and medical necessity determinations should be submitted by sending a written request for appeal using the level i provider.