Express Scripts Tier Exception Form
Express Scripts Tier Exception Form - Web follow the steps below when asking for a tiering exception: Web requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. Web the prescriber can complete a prior authorization electronically or via fax and explain why an exception is required. (1) formulary or preferred drugs contraindicated or tried and failed, or tried and not as effective as requested drug; Web request for formulary tier exception [specify below: Web log in don't have an account? You can ask us to make an exception to. If a drug has prior authorization (pa) or utilization management (um) requirements, then the pa or. Web if the member has tried and failed all the listed drugs or is unable to take the listed drugs for medical reasons, you can submit a formulary exception requesting coverage of the non. Prior authorization criteria is available upon.
Web 2020 national preferred formulary exclusions the excluded medications shown below are not covered on the express scripts drug list. Prior authorization criteria is available upon. Your prescriber may use the attached. Web express scripts is the pharmacy benefit manager for mutual of omaha rx and will be providing this service on behalf of mutual of omaha rx. Web please call us at 800.753.2851 to submit a verbal prior authorization request if you are unable to use electronic prior authorization. Web requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. Web tier exception coverage determination (for provider use only) drug & prescription information required (please write legibly) drug name:. (1) formulary or preferred drugs contraindicated or tried and failed, or tried and not as effective as requested drug; If you are charged a high copay at the pharmacy, talk to your pharmacist and your plan to find out why. Web if the member has tried and failed all the listed drugs or is unable to take the listed drugs for medical reasons, you can submit a formulary exception requesting coverage of the non.
Web follow the steps below when asking for a tiering exception: Web express scripts is the pharmacy benefit manager for mutual of omaha rx and will be providing this service on behalf of mutual of omaha rx. Your prescriber may use the attached. You can ask us to cover your. Web tier exception coverage determination (for provider use only) drug & prescription information required (please write legibly) drug name:. Express scripts makes the use of prescription drugs safer and more affordable. Web please call us at 800.753.2851 to submit a verbal prior authorization request if you are unable to use electronic prior authorization. Web request for formulary tier exception [specify below: Web once a decision has been made, express scripts will send a letter to the physician’s office and the member regarding the decision of the coverage determination. Web this form will allow you to request access to your protected health information (phi) that an express scripts entity maintains.
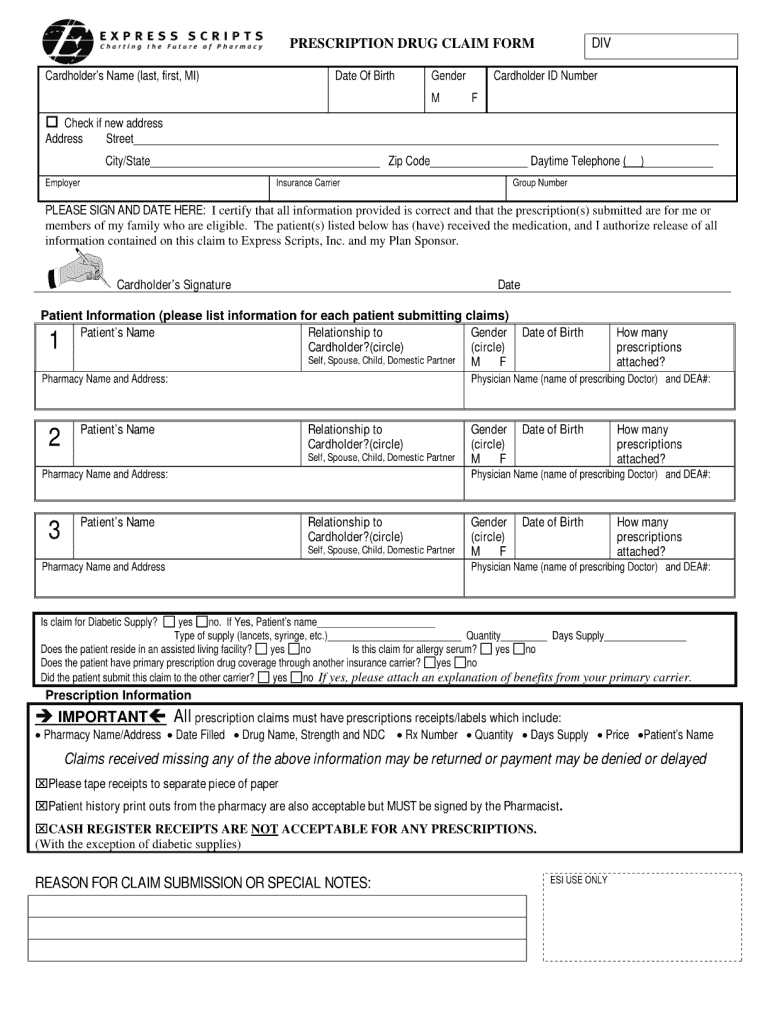
Express Scripts Fax Forms for Physicians Prior Authorization Fill Out
Complete copa y* (tie it is not necessary exception f ields. Web once a decision has been made, express scripts will send a letter to the physician’s office and the member regarding the decision of the coverage determination. Web express scripts is the pharmacy benefit manager for mutual of omaha rx and will be providing this service on behalf of.
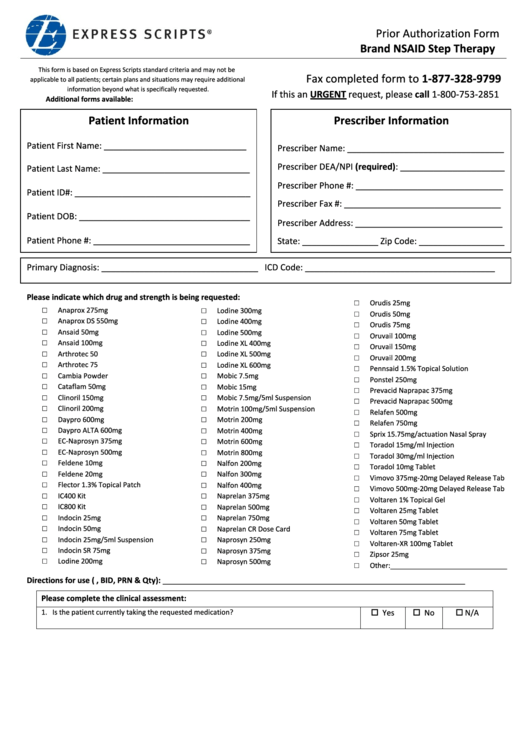
Express Scripts Prior Authorization Form Brand Nsaid Step Therapy
Web a prescriber supporting statement is required for tier exception requests. If a drug has prior authorization (pa) or utilization management (um) requirements, then the pa or. (1) formulary or preferred drugs contraindicated or tried and failed, or tried and not as effective as requested drug; Web if the member has tried and failed all the listed drugs or is.
ads/responsive.txt Aetna Medicare Tier Exception form Awesome Cigna
Prior authorization criteria is available upon. Your prescriber may use the attached. Web a prescriber supporting statement is required for tier exception requests. (1) formulary or preferred drugs contraindicated or tried and failed, or tried and not as effective as requested drug; Electronic requests can be done through portals such as.
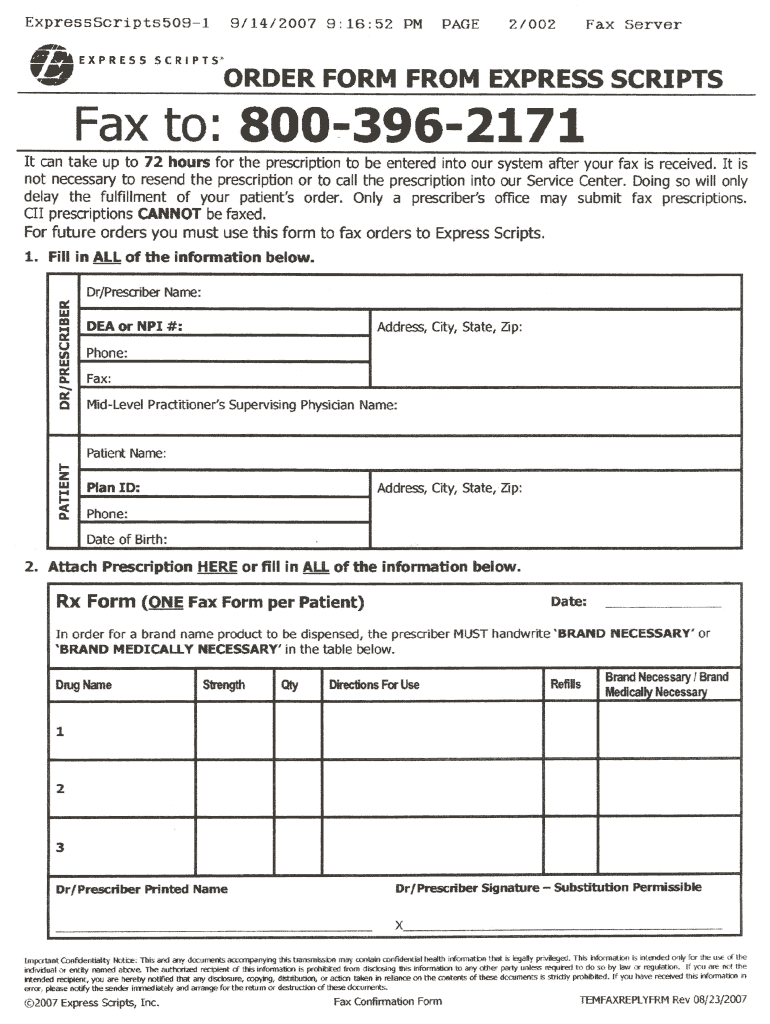
Order Form from Express Scripts 20072021 Fill and Sign Printable
You can ask us to cover your. Web once a decision has been made, express scripts will send a letter to the physician’s office and the member regarding the decision of the coverage determination. Web this form will allow you to request access to your protected health information (phi) that an express scripts entity maintains. Web tier exception coverage determination.
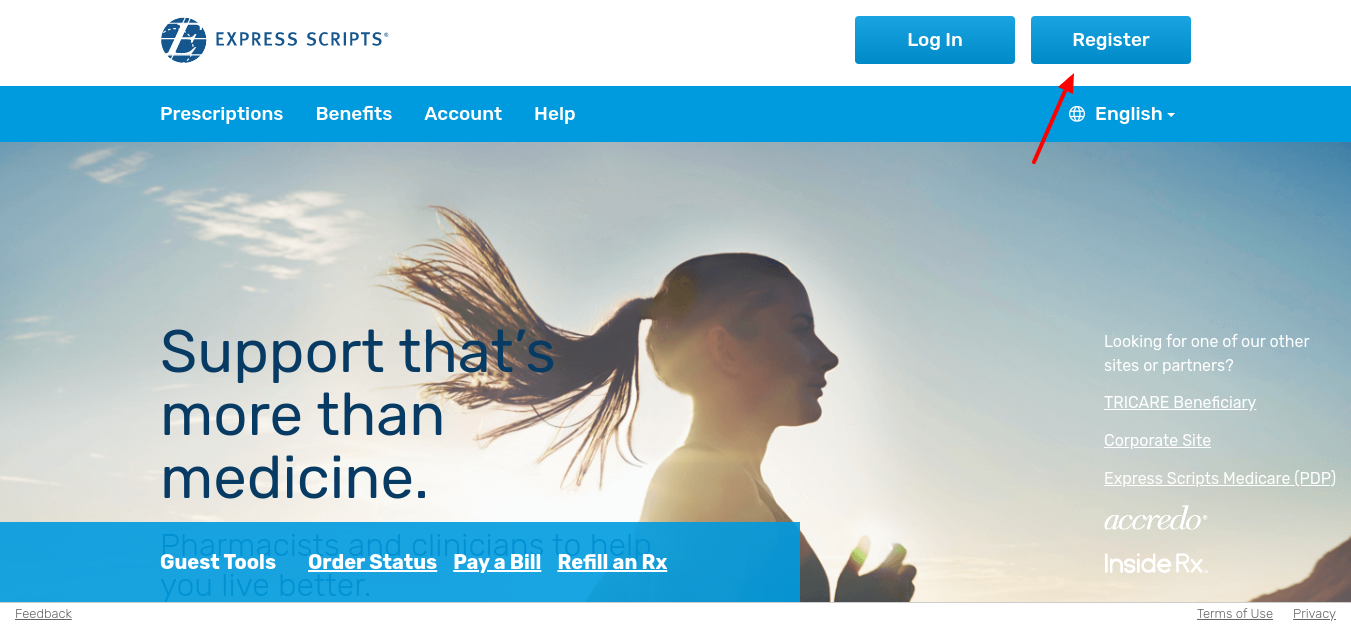
How to Register for Express Scripts For
Web request for formulary tier exception [specify below: Web a prescriber supporting statement is required for tier exception requests. Your prescriber may use the attached. Web log in don't have an account? Prior authorization criteria is available upon.
Care1st Prior Authorization Form
Web once a decision has been made, express scripts will send a letter to the physician’s office and the member regarding the decision of the coverage determination. Web requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. Register now we make it easy to share information get your written prescriptions to us.
Optum Rx Prior Authorization Form 11 Thefrenchteeshirt
If you are charged a high copay at the pharmacy, talk to your pharmacist and your plan to find out why. Specifically, this form allows you to request certain. If a drug has prior authorization (pa) or utilization management (um) requirements, then the pa or. Prior authorization criteria is available upon. Web 2020 national preferred formulary exclusions the excluded medications.
Express Scripts Tier Exception Form 2021 Fill Online, Printable
Web please call us at 800.753.2851 to submit a verbal prior authorization request if you are unable to use electronic prior authorization. Register now we make it easy to share information get your written prescriptions to us by using our mail order form. You can ask us to make an exception to. Request for a lower co pay (tieri to.
Aetna Medicare Tier Exception form Elegant Aco
Web the prescriber can complete a prior authorization electronically or via fax and explain why an exception is required. Your prescriber may use the attached. Web if the member has tried and failed all the listed drugs or is unable to take the listed drugs for medical reasons, you can submit a formulary exception requesting coverage of the non. Web.
ads/responsive.txt Aetna Medicare Tier Exception form Elegant top
(1) formulary or preferred drugs contraindicated or tried and failed, or tried and not as effective as requested drug; Web requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. Web log in don't have an account? Prior authorization criteria is available upon. Complete copa y* (tie it is not necessary exception f.
Web The Prescriber Can Complete A Prior Authorization Electronically Or Via Fax And Explain Why An Exception Is Required.
Web if the member has tried and failed all the listed drugs or is unable to take the listed drugs for medical reasons, you can submit a formulary exception requesting coverage of the non. Web please call us at 800.753.2851 to submit a verbal prior authorization request if you are unable to use electronic prior authorization. Web express scripts is the pharmacy benefit manager for mutual of omaha rx and will be providing this service on behalf of mutual of omaha rx. Prior authorization criteria is available upon.
Complete Copa Y* (Tie It Is Not Necessary Exception F Ields.
(1) formulary or preferred drugs contraindicated or tried and failed, or tried and not as effective as requested drug; You can ask us to cover your. Web this form will allow you to request access to your protected health information (phi) that an express scripts entity maintains. Your prescriber may use the attached.
Web Once A Decision Has Been Made, Express Scripts Will Send A Letter To The Physician’s Office And The Member Regarding The Decision Of The Coverage Determination.
Web tier exception coverage determination (for provider use only) drug & prescription information required (please write legibly) drug name:. Specifically, this form allows you to request certain. Web millions trust express scripts for safety, care and convenience. Web 2020 national preferred formulary exclusions the excluded medications shown below are not covered on the express scripts drug list.
Express Scripts Makes The Use Of Prescription Drugs Safer And More Affordable.
Electronic requests can be done through portals such as. Web request for formulary tier exception [specify below: You can ask us to make an exception to. Web requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information.