Medicare Botox Prior Authorization Form
Medicare Botox Prior Authorization Form - Health partnersr r kidzpartners r r please attach any pertinent medical history or information for this patient that may. Web botox uses various forms of botulinum toxin to temporarily paralyze muscle activity or block certain nerves. Page 2 of 2 (all fields must be completed and legible for precertification review) aetna. Web botox ® (onabotulinumtoxina) injectable medication precertification request. Web prior to botox, how many headache days per month is/was your patient experiencing? Web prior authorization prior authorization is a process through which a request for provisional affirmation of coverage is submitted for review before a service is. Web botox® prior authorization form this form may also be used for requests to exceed the maximum allowed units. Web effective for dates of service july 1, 2020, and after, providers must request prior authorization for the following hospital opd services: Form available on alaska medicaid’s medication prior. Web get medicare forms for different situations, like filing a claim or appealing a coverage decision.
Web health insurance plans | aetna Patient belongs to (please check one): Health partnersr r kidzpartners r r please attach any pertinent medical history or information for this patient that may. Web use of these botulinum toxin codes in conjunction/paired with procedure codes other than 64612 or 64615 will not require prior authorization under this program. Web prior to botox, how many headache days per month is/was your patient experiencing? If the hopd initiates the authorization process, can the performing physician/clinician submit clinical/medical documentation directly to novitas separately? Prior authorization for the initial five services (blepharoplasty, botulinum toxin injections, panniculectomy, rhinoplasty, and vein ablation) started on june 17, 2020, for dates of. Web prior authorization prior authorization is a process through which a request for provisional affirmation of coverage is submitted for review before a service is. Web medicare provides coverage when botox injections are being used to treat any of these conditions listed above. This service category will be in.
Web opd providers can start submitting the prior authorization requests on june 15, 2023, for dates of service on or after july 1, 2023. Web prior to botox, how many headache days per month is/was your patient experiencing? Web pharmacy resources prior authorization forms prior authorization for professionally administered drugs submitting a prior authorization request prescribers should. Web how they work. Patient belongs to (please check one): Web health insurance plans | aetna Aside from its cosmetic use, botox injections have been approved by the. Page 2 of 2 (all fields must be completed and legible for precertification review) aetna. Web botox ® (onabotulinumtoxina) injectable medication precertification request. Web medicare allows coverage and payment for only those services that are considered to be reasonable and necessary for the diagnosis or treatment of illness or.
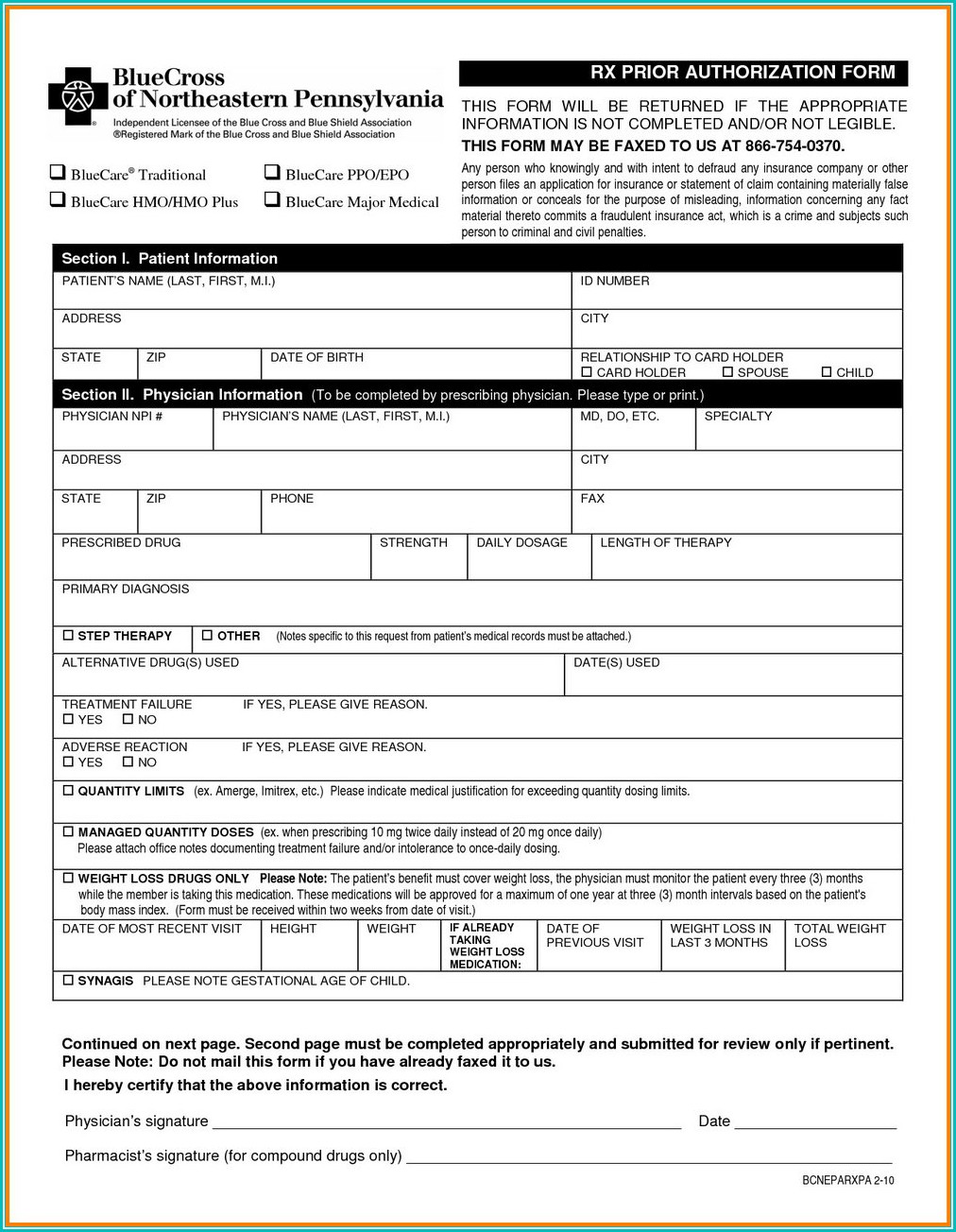
Prior Authorization Form For Medicare Part B Form Resume Examples
This service category will be in. Web medicare provides coverage when botox injections are being used to treat any of these conditions listed above. Health partnersr r kidzpartners r r please attach any pertinent medical history or information for this patient that may. Aside from its cosmetic use, botox injections have been approved by the. Web opd providers can start.
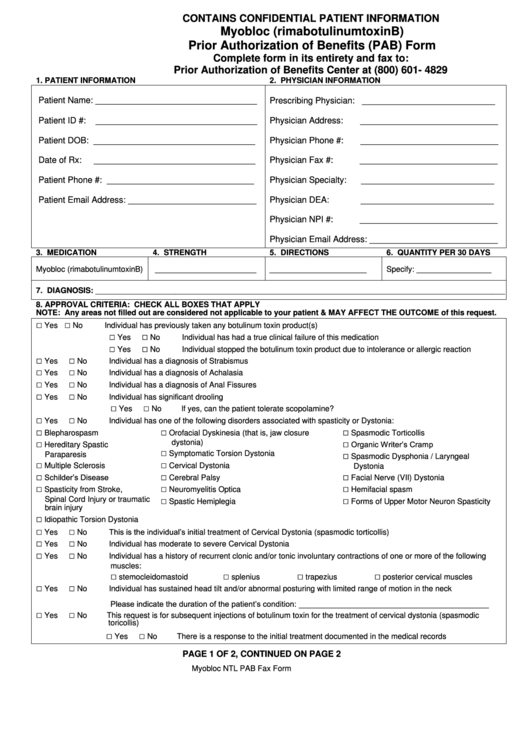
Myobloc (Rimabotulinumtoxinb) Prior Authorization Of Benefits (Pab
Form available on alaska medicaid’s medication prior. Web botox® prior authorization form this form may also be used for requests to exceed the maximum allowed units. However, it’s a good idea to get preauthorization. Web botox uses various forms of botulinum toxin to temporarily paralyze muscle activity or block certain nerves. Web how they work.
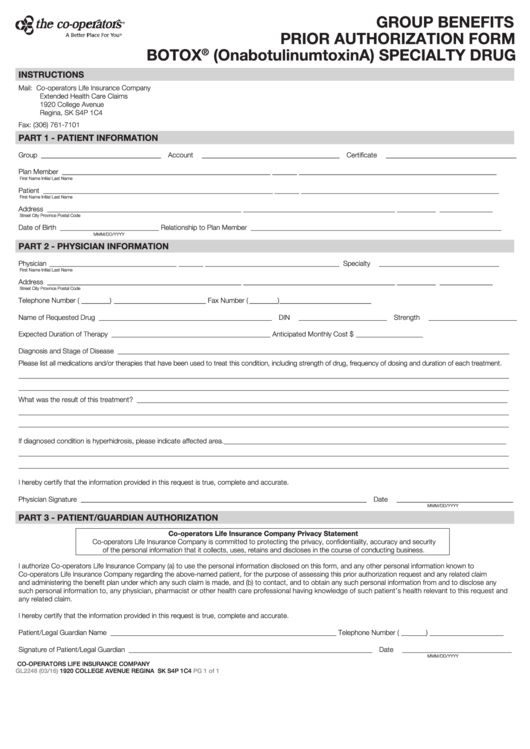
Fillable Form Gl2248 Group Benefits Prior Authorization Botox
Health partnersr r kidzpartners r r please attach any pertinent medical history or information for this patient that may. Web medicare provides coverage when botox injections are being used to treat any of these conditions listed above. Web medicare allows coverage and payment for only those services that are considered to be reasonable and necessary for the diagnosis or treatment.
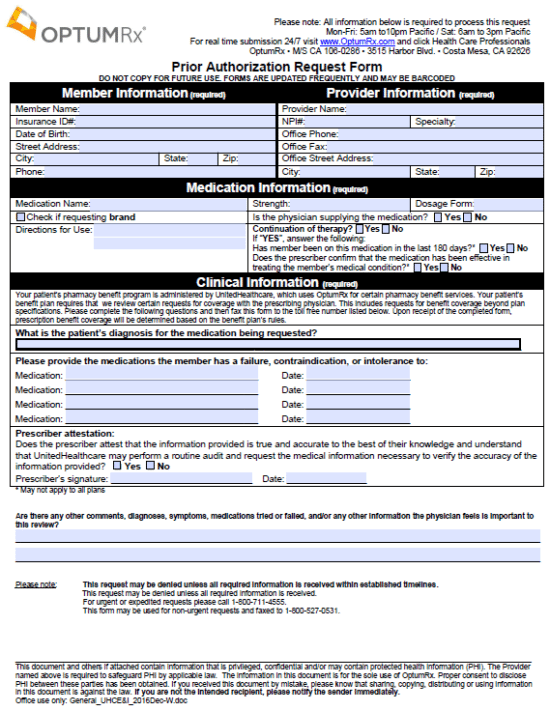
Optumrx Prior Authorization Form Cialis optumrx prior authorization
Web health insurance plans | aetna Web use of these botulinum toxin codes in conjunction/paired with procedure codes other than 64612 or 64615 will not require prior authorization under this program. Web botox® prior authorization form this form may also be used for requests to exceed the maximum allowed units. Form available on alaska medicaid’s medication prior. Web pharmacy resources.
Standard Pharmacy Prior Authorization Form for Prepaid Health Plans
Web botox uses various forms of botulinum toxin to temporarily paralyze muscle activity or block certain nerves. Web get medicare forms for different situations, like filing a claim or appealing a coverage decision. However, it’s a good idea to get preauthorization. Web botox® prior authorization form this form may also be used for requests to exceed the maximum allowed units..
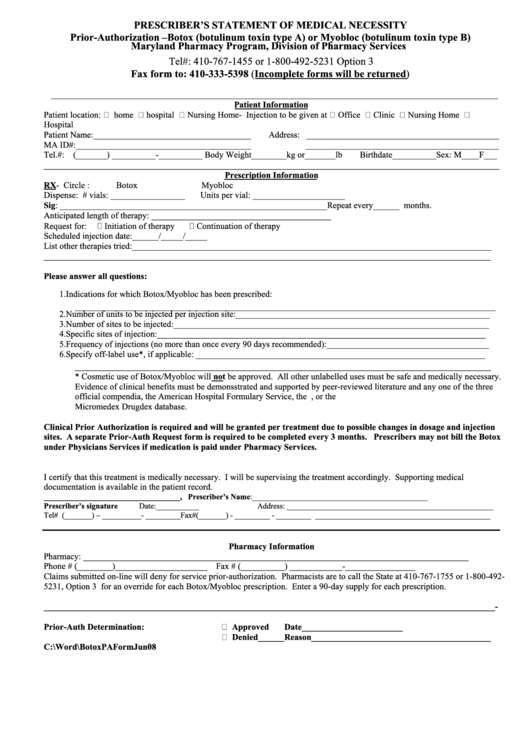
Botox Or Myobioc Prior Authorization Form Prescriber'S Statement Of
Web medicare provides coverage when botox injections are being used to treat any of these conditions listed above. Web how they work. Web effective for dates of service july 1, 2020, and after, providers must request prior authorization for the following hospital opd services: Aside from its cosmetic use, botox injections have been approved by the. However, it’s a good.
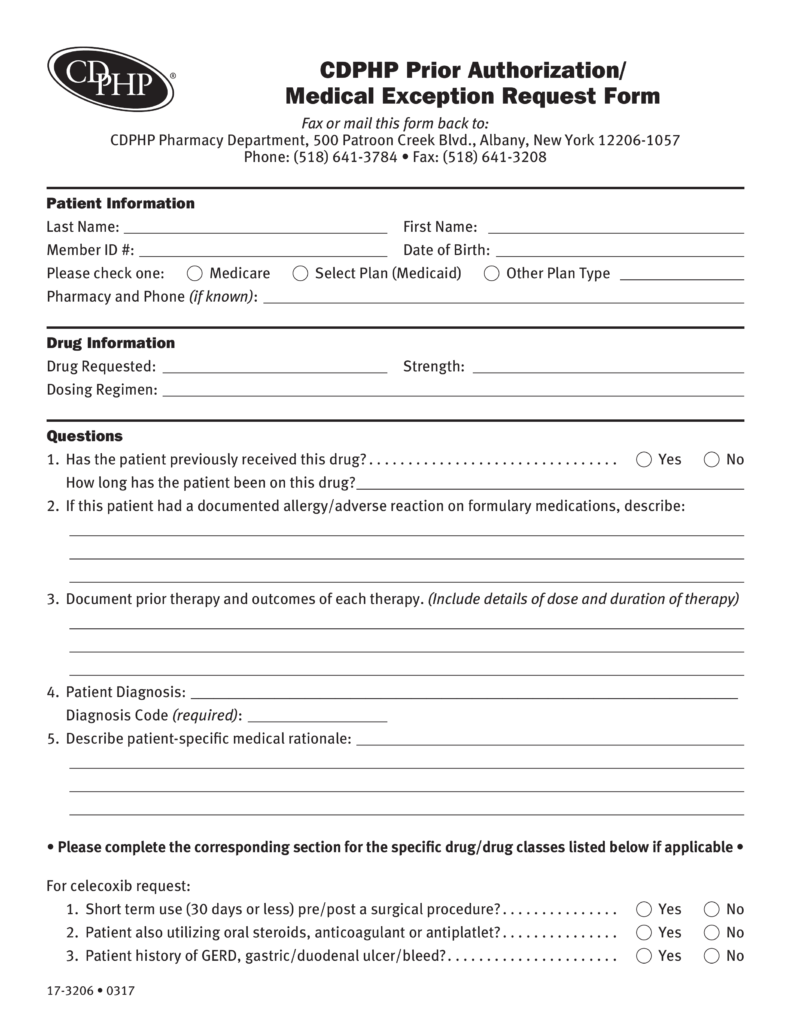
Free CDPHP Prior (Rx) Authorization Form PDF eForms
If the hopd initiates the authorization process, can the performing physician/clinician submit clinical/medical documentation directly to novitas separately? Web effective for dates of service july 1, 2020, and after, providers must request prior authorization for the following hospital opd services: Web botox® prior authorization form this form may also be used for requests to exceed the maximum allowed units. Web.
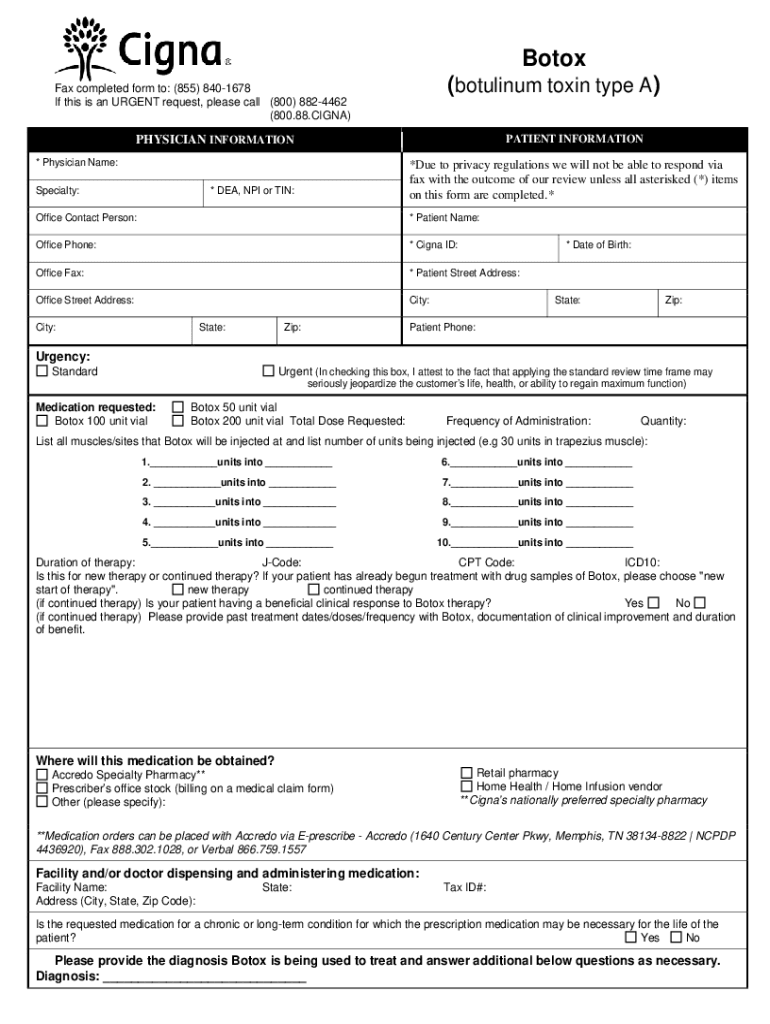
Cigna Botox Prior Authorization Form Fill Out and Sign Printable PDF
Web use of these botulinum toxin codes in conjunction/paired with procedure codes other than 64612 or 64615 will not require prior authorization under this program. Web prior to botox, how many headache days per month is/was your patient experiencing? This service category will be in. Web botox uses various forms of botulinum toxin to temporarily paralyze muscle activity or block.
Medicare Part D Prior Authorization form for Medication Lovely Arkansas
Web botox uses various forms of botulinum toxin to temporarily paralyze muscle activity or block certain nerves. Web botox® prior authorization form this form may also be used for requests to exceed the maximum allowed units. If the hopd initiates the authorization process, can the performing physician/clinician submit clinical/medical documentation directly to novitas separately? Web how they work. Web use.
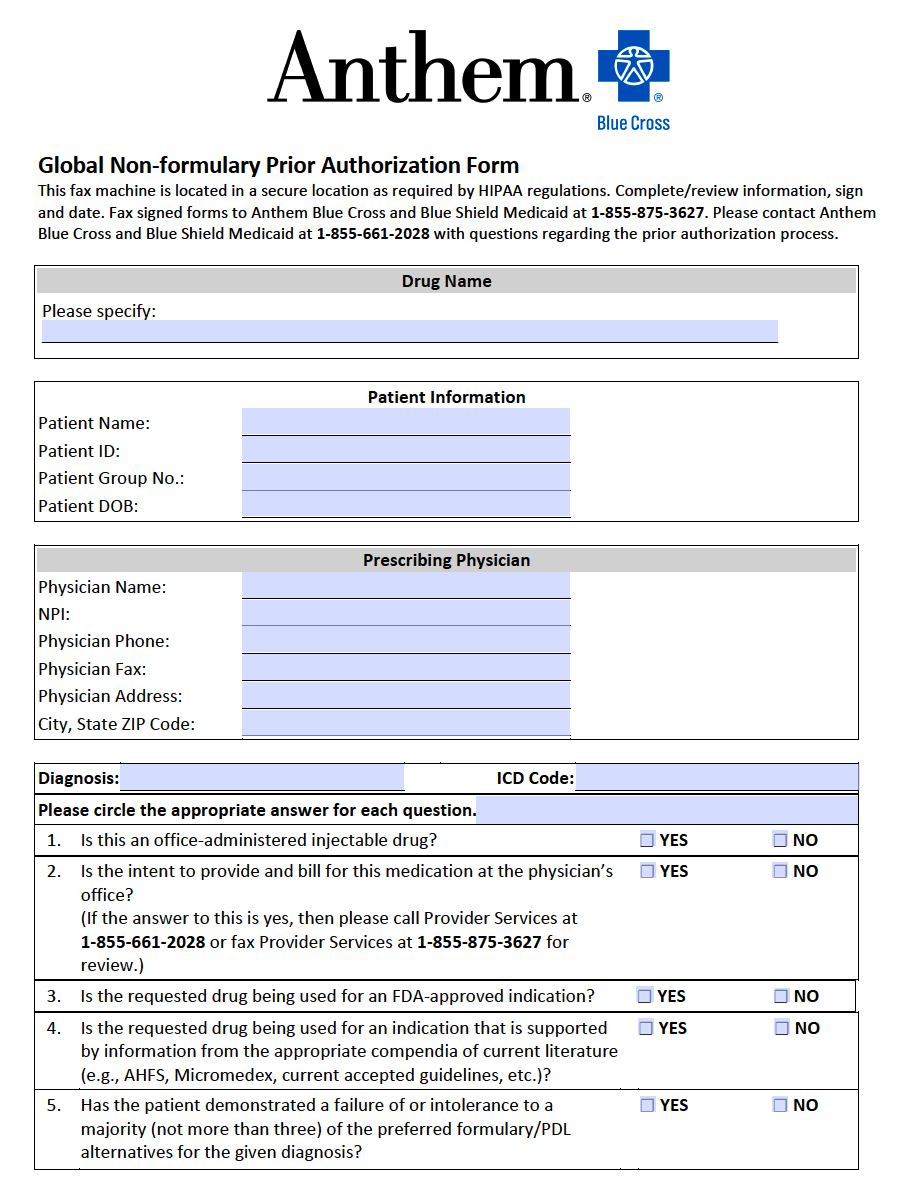
Free Anthem Blue Cross / Blue Shield Prior Prescription (Rx
Web effective for dates of service july 1, 2020, and after, providers must request prior authorization for the following hospital opd services: Web botox uses various forms of botulinum toxin to temporarily paralyze muscle activity or block certain nerves. However, it’s a good idea to get preauthorization. If the hopd initiates the authorization process, can the performing physician/clinician submit clinical/medical.
Web Medicare Allows Coverage And Payment For Only Those Services That Are Considered To Be Reasonable And Necessary For The Diagnosis Or Treatment Of Illness Or.
Patient belongs to (please check one): This service category will be in. Aside from its cosmetic use, botox injections have been approved by the. Web use of these botulinum toxin codes in conjunction/paired with procedure codes other than 64612 or 64615 will not require prior authorization under this program.
Health Partnersr R Kidzpartners R R Please Attach Any Pertinent Medical History Or Information For This Patient That May.
Web botox ® (onabotulinumtoxina) injectable medication precertification request. Web pharmacy resources prior authorization forms prior authorization for professionally administered drugs submitting a prior authorization request prescribers should. Page 2 of 2 (all fields must be completed and legible for precertification review) aetna. Prior authorization for the initial five services (blepharoplasty, botulinum toxin injections, panniculectomy, rhinoplasty, and vein ablation) started on june 17, 2020, for dates of.
If The Hopd Initiates The Authorization Process, Can The Performing Physician/Clinician Submit Clinical/Medical Documentation Directly To Novitas Separately?
Web botox® prior authorization form this form may also be used for requests to exceed the maximum allowed units. Web health insurance plans | aetna Web medicare provides coverage when botox injections are being used to treat any of these conditions listed above. Web how they work.
However, It’s A Good Idea To Get Preauthorization.
Web effective for dates of service july 1, 2020, and after, providers must request prior authorization for the following hospital opd services: Form available on alaska medicaid’s medication prior. Web botox uses various forms of botulinum toxin to temporarily paralyze muscle activity or block certain nerves. Web opd providers can start submitting the prior authorization requests on june 15, 2023, for dates of service on or after july 1, 2023.